The fact that injuries to the eye and its surrounding region demand special attention and create great concern for patient and doctor is self-evident when the eye alone is involved, but when other life-threatening injuries are present, the eye injury, seeming slight at the time, might be overlooked. Sometimes, the eyelids might be so swollen that it is difficult to examine the eyes and a serious perforating injury could be obscured.When other injuries are present and an anaesthetic is needed, it is essential that the eyes are examined carefully, if possible under
the same anaesthetic. As in the case of injuries elsewhere, those to the eye demand urgent and immediate treatment, and neglect can result in tragedy even though the problem might have at first seemed slight.
Injuries to the Globe
Contusion
The eye casualty officer comes to recognize a familiar pattern of contusion, the effect of squash ball injuries and blows from flying objects in industry or after criminal assault. The extent of damage to the eye from contusion depends on whether it has been possible to close the eyelids in time before the moment of impact. If the lids have been closed, bruising and swelling of the eyelids is marked and the injury to the eye might be minimal. The eyes themselves must always be
carefully examined, even when there is extreme swelling of the lids. It is always possible to examine an eye, if necessary using an eye speculum under general anaesthesia.The important clinical features of contusion injury are best considered by looking at the anatomical parts of the eye.
Cornea
The most common injury to the cornea is the corneal abrasion. Here, the patient
experiences a sharp pain in the eye in the early morning usually on waking, sometimes many months after the initial injury. The cornea is to be examined carefully with the slitlamp biomicroscope. This problem of recurrence is a reason to treat these abrasions with some care and to provide the patient with a lubricating
ointment to be used at night for some time after the original injury has healed. Sometimes, recurrent abrasion results from a rare inherited disorder of the corneal epithelium. When a patient presents with a corneal abrasion, the eyelids are often swollen perhaps from rubbing and the distress and agitation can be considerable. Examination may be impossible without first instilling a drop of local anaesthetic.
These drops should never be continued as treatment because they could seriously delay the healing of the cornea.
Anterior Chamber
A small bleed into the anterior chamber of the eye is seen as a fluid level of blood inferiorly (“hyphaema”). This is a sign of potential problems because of the risk of secondary bleeding after two or three days. This risk is especially serious in children and the complication can lead to secondary glaucoma and at worst, the loss of the eye.The parents need to be warned about this if there is a hyphaema. Treatment is by strict rest with little or no head movement to avoid further bleeding and regular measurement of the intraocular pressure.
Iris
When confronted by a flying missile, the normal reaction is to attempt to close the eyelids and to rotate the eyes upward. This is the reason why the commonest point of impact is the lower temporal part of the eye and it is in this region of the iris that one is most likely to see peripheral iris tears (“iridodialysis”). When the eye is compressed the iris periphery is torn at its root, leaving a crescentic gap, which looks black, but through which the fundus and red reflex can be observed. Such an injury also provides an excellent view of the peripheral part of the lens and the zonular ligament
Contusion can result not in a tear of the iris root, but in a tangential splitting of the iris and ciliary body from the sclera producing recession of the angle of the anterior chamber; the appearance is often associated with secondary glaucoma, sometimes many years after the injury and is identified using the special contact lens known as the gonioscope. A sudden impact on the eye can also produce microscopic radial tears in the pupillary sphincter of the iris. This could be a subtle microscopic sign of previous injury when no other signs are present, or the damage might be more severe, resulting in persistent dilatation of the pupil (traumatic mydriasis). Unless the eye is examined, this widening of the pupil after injury can be mistaken for a third cranial nerve palsy.
Lens
Any severe contusion of the eye is liable to cause traumatic cataract(in rossette shaped pattern), but the lens might not become opaque for many years after the injury. The lens can also become subluxated (slightly displaced because of partial rupture of the zonular ligament) or even dislocated either anteriorly into the anterior chamber or posteriorly into the vitreous.
Vitreous
The vitreous can become displaced from its attachments around the processes of the ciliary body or around the optic disc after a contusion injury if it has not already undergone this change as part of the normal ageing process. The patient might be aware of something floating in front of the vision. More extensive floating black spots can indicate a vitreous haemorrhage caused by excessive vitreous traction on a retinal blood vessel. Although such haemorrhages usually clear completely in time, they tend to accompany more serious damage to the retina,which can only be fully revealed once clearing has taken place.
Retina
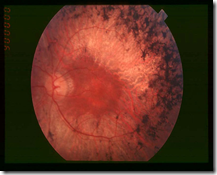
Bruising and oedema of the retina are seen as grey areas with scattered haemorrhages. The macular region is susceptible to oedema after contusion injuries, causing permanent damage to the reading vision. Just as tears can occur to
the peripheral iris, so a similar problem is seen in the peripheral retina. These crescent-shaped retinal dialyses are also most common in the lower temporal quadrant and their importance lies in the fact that they may lead to a detachment of the retina unless the tear is sealed by laser treatment. Any significant contusion injury of the eye requires a careful inspection of the peripheral retina.
Choroid
Tears in the choroid following contusion have a characteristic appearance. They are concentric with the disc and are seen as white crescents where the sclera is exposed. When near the macula, there is usually permanent damage to the central vision. They are also potential sites for choroidal neovascularisation.
Optic Nerve
A variable degree of optic atrophy can become apparent a few weeks after a contusion injury. Blunt injuries to the eye can cause bleeding into the optic nerve sheath or tearing of the tiny pial blood vessels that supply the nerve, both resulting in complete, irreversible loss of vision on the affected side. Attempts have been made to relieve the situation by emergency decompression of the optic nerve, nerve sheath fenestration, use of hyperbaric oxygen and highdose steroids. No treatment has shown a clear benefit except optic nerve decompression in specific circumstances.
Perforation
As soon as the globe of the eye is penetrated, there is a serious risk of infection. The vitreous is an excellent culture medium and in the pre-antibiotic era, eyes were totally lost within two or three days as a result of this. A perforating wound of the eye must, therefore, be considered a surgical emergency. Perforating injuries are seen in children from scissor blades, screwdrivers, darts and other more bizarre objects. In adults, there has been a dramatic fall in the incidence of such injuries since the introduction of compulsory seat belts but “do-it-yourself” accidents and assaults still take their toll. Following such an injury it is important to consider the possibility of an intraocular foreign body, especially when there is a history of using a hammer and chisel. The outcome of a perforating injury is dependent on the depth of penetration and the care with which the wound is cleaned and sutured. If the cornea alone is damaged, excellent results can be obtained by careful suturing under general anaesthesia using the operating microscope. If the lens has been damaged, early cataract surgery might be needed and deeper penetration can result in the need for retinal detachment surgery. On admission or in the casualty department, the patient is given tetanus prophylaxis and both systemic and local antibiotics. If early surgery under general anaesthesia is likely to be needed, it is better for the patient not to eat or drink to avoid delays in hospital. If it becomes clear that the injury is a serious one, it is better to warn the patient at an early stage about the possible risk of losing the sight of the eye or even the need to replace it with an artificial one.
Intraocular Foreign Body
Metallic foreign bodies tend to enter the eyes of those who operate high-speed grinders without goggles or those using a hammer and chisel on metal without eye protection. These injuries might seem slight at first and sometimes patients do not attach much importance to them.Any such eye injury with this occupational history warrants an X-ray of the eye. When ferrous metals remain in the eye they can cause immediate infection, or at a later date the deposition of ferrous salts, in a process known as siderosis. This can eventually lead to blindness of the eye. Other metals also tend to give reactions, particularly copper and for this reason the metallic fragment should be removed. This is achieved either by using intravitreous forceps under microscopic control or using a magnet. The exact surgical technique is planned beforehand once the foreign body has been accurately localised in the eye. Airgun pellets cause particularly severe eye injuries and the eye is often lost because of the extensive disruption at the time of the injury. Some intraocular foreign bodies, such as glass particles or some alloys, might be tolerated quite well and a decision could have to be made as to whether observation is preferable in the first instance. This especially applies when the sight of the eye remains good.When a foreign body is not to be removed immediately, many ophthalmologists would insert intravitreal antibiotics as a prophylactic measure against endophthalmitis. When a foreign body is found lying deeply in the cornea, its removal can result in loss of aqueous and collapse of the anterior chamber. It is prudent to arrange that removal should be done under full sterile conditions in the operating theatre, where the corneal wound can be sutured if necessary.
Sympathetic Ophthalmia
This rare complication of perforation is more common in children. The injured eye remains markedly inflamed and the wound might have been cleaned inadequately or too late. Over a period of two weeks to several months or even years a particular type of inflammatory response begins in the uvea and subsequently a similar reaction occurs in the other eye. The inflammation in both eyes can be so severe as to cause blindness. The condition does, however, respond well to steroid treatment and it is extremely rare. Occasionally, one sees patients who have an artificial eye complaining of transient blurring of the vision of their remaining eye. They need to be examined carefully for signs of uveitis.
Injuries to the Eyelids
Loss or destruction of eyelid tissue should always be treated as a threat to vision. The upper lid especially is important in this respect. The immediate concern is to ensure that the cornea is properly covered when the eyelids are closed. If more than one-third of the margin of the upper lid is lost, this must be replaced by grafting from the lower lid.When less than one-third is missing, the gaping wound can usually be closed directly. Up to one-third of the lower lid can also be closed by direct suturing. When more than this is lost or when it has been transferred to the upper lid, a slide of tissue from the lateral canthus can be effected, combined if necessary with a rotating cheek flap. One of the most important features of the repair of lid injuries is the method of suturing. If the lid margin is involved, the repair should be made using the operating microscope and the fine suture material available in an eye department. An untidy repair can result in a permanently watering eye because of kinking of the eyelid. This interferes with the proper moistening of the cornea during blinking or when asleep. Special attention must be
paid when the medial part of the eyelid has been torn, as this contains the lacrimal canaliculus. Again, unless repair is carried out using an accurate technique under general anaesthesia in theatre, the risk of a permanently watering eye is increased.
Injuries to the Orbit
The most common type is the “blow-out fracture”. Here the globe and contents of the orbit are forced backwards, causing fracture of the orbital floor and displacement of bone downwards into the antrum of the maxillary sinus. The inferior rectus muscle becomes tethered in the wound so that there is mechanical limitation of upward movement. The infraorbital nerve, which traverses the orbital floor, can also be injured, producing anaesthesia of the skin of the cheek. Once the surrounding swelling has subsided, the posterior displacement of the globe becomes
obvious and the globe of the eye itself often shows evidence of contusion. A considerable improvement from the functional and cosmetic point of view can be obtained by positioning a plastic or Teflon implant in the floor of the orbit after freeing the prolapsed tissue. Fractures of the skull that extend into the orbit can be accompanied by retro-orbital haemorrhage and proptosis.Cranial nerve palsies affecting the ocular movements are also commonly seen in this type of injury and the vision can be affected by optic nerve damage.A blow on the eye can result in sudden blindness with at first no other evidence of injury (apart from an afferent pupillary defect), but subsequently, the optic disc becomes pale and atrophic after two or three weeks.
 Chalazion, also known as a meibomian gland lipogranuloma, is a
Chalazion, also known as a meibomian gland lipogranuloma, is a